Clinical registries
What is a clinical registry?
A clinical registry is a national database that records clinical and patient outcomes for a specific disease or service area. This data is used to monitor and improve care and outcomes for patients both at a national level and at individual facilities. Over time, the aim of a clinical registry is to help improve outcomes for all patients within the registry’s focus area.
Clinical registries are usually developed by groups of research and health care professionals. They are typically independent of the health care system (i.e. they are not created or managed by hospitals) and can be based in universities or other independent organisations. Any organisation that runs a clinical registry should also have an independent governance structure to guide its data collection and clearly articulate how any data it collects will be used.
Examples of how clinical registry data may be used include:
- Establishing and supporting national benchmarks (i.e. to compare the performance of services that treat the same conditions against each other and establish a national “average”).
- Improving understanding of factors that lead to clinical variation (i.e. different results for different patients).
- Improving the effectiveness of care.
- To conduct population-based research projects.
Studies have shown that participation in clinical registries can contribute to improvements in consistency and quality of care. Participation is voluntary and will not affect your care. You can opt out at any time by following the instructions provided.
What is Ramsay doing in this area?
Ramsay Health Care supports participation in clinical registries and has actively sought to contribute to registries in key priority areas. As an organisation, we seek to work with clinical registries to better understand our services and ensure that we are working with our doctors, nurses and allied health professionals to continually improve outcomes for our patients.
There are currently 31 national clinical registries listed by the Australian Safety and Quality Commission.
How do clinical registries improve the quality of care at Ramsay?
Ramsay Health Care participates in 26 clinical registries. We work with each registry to develop Ramsay-specific reports that can be used to identify outcomes for our patients. Based on the findings of these reports, we then actively work with our doctors, nurses and allied health professionals at each location to understand how we are performing and the ways in which we can continue to improve our patients’ outcomes and the quality of their care.
Listed below are some of the clinical registries Ramsay participates in.
Click the plus sign (+) on the right side of any heading to expand and view more information.
Bariatric Surgery Registry
The primary aim of the Bariatric Surgery Registry is to measure outcomes for patients undergoing bariatric surgery across public and private hospitals in Australia and New Zealand. It was established in 2009 and is part of the School of Public Health and Preventative Medicine at Monash University.
The registry has collected information from more than 90,000 patients who have undergone bariatric surgery and Ramsay is pleased to support it.
How does participation in this registry assist patients?
Participation in the registry enables Ramsay to track the outcomes of patients undergoing surgery in our hospitals. The primary aim of the registry is to measure the quality and safety of bariatric procedures. This data can be used to:
- Confirm patient outcomes from bariatric surgery at a community level.
- Measure the change in diabetes status over time in this population.
- Translate these efficacy and health outcomes into practice guidelines.
- Make the registry a resource for future research projects.
What if I don’t want my information to be included in the registry?
Any patient who is eligible for participation in the Bariatric Surgery Registry will be notified by their surgeon and provided with a comprehensive information sheet prior to any surgery being performed. This sheet explains what the registry is, what data is collected for it, and how that data could be used. If a patient does not wish to have their data added to the registry, they are able to opt out by following instructions provided in the sheet.
Australian and New Zealand Society of Cardiac and Thoracic Surgeons
The Australian and New Zealand Society of Cardiac and Thoracic Surgeons (ANZSCTS) Database was created in 2001 and initially collected data on cardiac surgeries performed in Victorian hospitals. It expanded to a national program in 2007.
The ANZSCTS registry was established to create a standardised system for collecting data relating to patient outcomes following cardiac surgeries. This led to the identification of key performance indicators (KPIs), which contributed to the development of local standards. Today, these standards are used to benchmark individual and unit performance across Australia and New Zealand.
The ANZSCTS database is funded by the Victorian Department of Health, NSW Clinical Excellence Commission (CEC), Queensland Health and participating units. It has captured data from more than 150,000 surgeries, and there are 41 participating sites around Australia. All Ramsay Health Care facilities that perform cardiac procedures contribute data to this registry.
How does participation in this registry assist patients?
Participation in the registry enables Ramsay to track the outcomes of patients undergoing surgery in our hospitals. The registry aims to collect information on all adults having heart surgery in Australia and New Zealand and seeks to monitor and improve the results of cardiac procedures. By collecting and analysing this data, the steering group is able to monitor treatment and determine what procedures and techniques produce the best outcomes. This enables any doctors, nurses or hospitals that perform cardiac surgery to ensure they achieve the best possible outcomes for patients.
How do Ramsay outcomes compare?
View cardiac procedures graph.
In 2018-19, 1,555 cardiac surgical procedures were reported to the ANZSCTS Database by Ramsay Health Care.
The ANZSCTS Database uses an all-procedures risk-adjustment model. In 2018-19, all Ramsay Health Care units had risk-adjusted mortality rates that were lower than the predicted mortality (PM) rates. All eight units were within the 95% control limit (CL) on funnel plot analyses for risk-adjusted mortality rate (RAMR) amongst the Ramsay Health Care cohort. The average RAMR was 0.2% for Ramsay Health Care units and 0.9% for the national cohort.
What if I don’t want my information to be included in the registry?
Any patient who is eligible for participation in the ANZSCTS database will be notified by their surgeon and provided with a comprehensive information sheet prior to any surgery being performed. This sheet explains what the registry is, what data is collected for it, and how that data could be used. If a patient does not wish to have their data added to the registry, they are able to opt out by following instructions provided in the sheet.
Australasian Rehabilitation Outcomes Centre
The Australasian Rehabilitation Outcomes Centre (AROC) is the national registry for rehabilitation medicine in Australia and New Zealand. It is a joint initiative of the Australian rehabilitation sector and has been developed by care providers, funders, regulators and consumers. The registry commenced operations on 1 July 2002. With the support of its industry partners, AROC was established by the Australasian Faculty of Rehabilitation Medicine (AFRM) of the Royal Australasian College of Physicians (RACP).
How does participation in this registry assist patients?
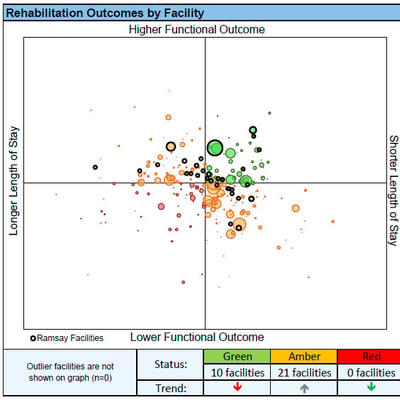
AROC delivers a national benchmarking system that can be used to improve rehabilitation outcomes in both the public and private sectors. The registry works with Ramsay on an annual basis to identify patient outcomes within each facility. Outcomes are assessed by functional independence measure (FIM) score and length of stay, and are risk-adjusted based on the types of patients admitted to our facilities.
AROC also works with Ramsay facilities to provide education, training and certification in FIM and other outcome measures, and regularly provides advice to Ramsay facilities on how their outcomes could be improved.
How do Ramsay outcomes compare?
The following graph demonstrates the performance of Ramsay Health Care Rehabilitation facilities based on improvement in functional outcomes (FIM score) and length of stay.
View rehabilitation outcomes graph.
This figure covers the period of 1 Jan 2019 – 30 Dec 2019. Circles ringed in black represent Ramsay facilities.
We aim to have all of our facilities in the top two quadrants, as they represent the achievement of higher functional outcomes. Ideally our facilities would achieve optimal functional outcomes with minimal hospitalisation. Facilities that achieve this are represented in the top right-hand quadrant and are coloured in green. Facilities that have lower than average functional outcomes and longer than average hospital stays are shown in red in the bottom left quadrant.
Ramsay does not have any facilities in this quadrant.
What if I don’t want my information to be included in the registry?
All rehabilitation hospitals around Australia participate in AROC and are required to contribute data. If a patient does not wish to have information contributed to AROC they should speak to a hospital executive.
National Joint Replacement Registry
The National Joint Replacement Registry is an initiative of the Australian Orthopaedic Association (AOA). The AOANJRR was established in 1999 with the aim of improving and maintaining the quality of care for individuals undergoing joint replacement surgery. Information on hip, knee, shoulder, elbow, wrist, ankle and spinal disc replacement is collected from all hospitals in Australia that perform these surgeries.
The AOANJRR is one of the largest clinical quality registries in Australia, with almost 1.5 million joint replacements recorded by the end of 2018. In 2018 alone, 122,500 procedures were recorded.
How does participation in this registry assist patients?
The AOANJRR is one of the few registries in Australia that has a 100% participation rate, with all orthopaedic surgeons participating. The registry continually monitors the performance of prosthesis combinations, and its publicly available annual report publishes information about poor-performing prosthesis. This has led to all prosthesis combinations being removed from the Australian market.
The registry also actively works with orthopaedic surgeons and facilities to ensure that they are supported in their efforts to improve patient outcomes.
How do Ramsay outcomes compare?
The following graphs show the performance of 16 Ramsay Health Care facilities that contribute data to the AOANJRR. These graphs are based on a 5-year reporting period between 2013 - 2018.
Cumulative Percent Revision of Primary Total Conventional Hip Replacement by Hospital (All Diagnoses, Excluding Large Head (>32mm) Metal/Metal)
Cumulative Percent Revision of Primary Total Knee Replacement by Hospital (All Diagnoses)
While all orthopaedic surgeons and Ramsay facilities contribute data to the registry, Ramsay only obtains facility reports from consenting orthopaedic surgeons. We then work with the AOANJRR to examine this data to ensure we achieve optimal outcomes for our patients.
What if I don’t want my information to be included in the registry?
Any patient who is eligible for participation in the AOANJRR database will be advised by their orthopaedic surgeon and will receive a comprehensive information sheet. This sheet explains what the registry is, what data is collected for it, and how that data could be used. If a patient does not wish to have their data added to the registry, they are able to opt out by following instructions provided in the sheet.
Australian and New Zealand Intensive Care Society Registry
The Australian and New Zealand Intensive Care Society (ANZICS) maintains a series of clinical registries that are designed to track outcomes of patients who are admitted into intensive care units. Ramsay Health Care participates in two of these registries: the ANZICS Adult Patient Database and the ANZICS Critical Care Resource survey.
The ANZICS Adult Patient Database collects outcome data for every adult patient admitted to an intensive care unit in Australia. All Ramsay Hospitals participate in the APD and regularly contribute data. The ANZICS Critical Care Resource survey is a database that tracks ICU capacity around Australia. Its data is collected through an annual survey.
The ANZICS APD is one of the largest ICU-related databases in the world, with more than 2 million patient episodes recorded. The database has been used for more than ten years to benchmark and track outcomes of patients who were admitted to Australian ICUs and has been instrumental in improving patient outcomes during that time.
The ANZICS CCR was established in 1993 and data is currently collected from 80% of all ICUs in Australia. The CCR database was an invaluable tool for managing resources during the COVID-19 pandemic.
How does participation in this registry assist patients?
The ANZICS APD is used to monitor ICU performance around Australia. It does this by routinely collecting, analysing and publishing de-identified data from contributing ICUs. ANZICS then works with the ICU community to use this information to improve care and outcomes for critically ill patients. This is achieved by sharing data and insights via regular publications and working with individual units when required. Through this, ANZICS helps ensure high standards for ICU patient care and the continued improvement of ICU patient outcomes.
How do Ramsay outcomes compare?
The following funnel plot shows the performance of 13 Ramsay Health Care facilities that contribute data to the APD. Any facilities that are outside of the solid lines are outliers, which means their outcomes are significantly different from other facilities. The Ramsay facilities are marked with red stars and none are considered outliers.
View ANZICS standardised mortality ratios graph.
The following graph shows the efficiency of individual ICUs by plotting the ANZROD Standardised Mortality Ratio against the Risk-Adjusted Length of Stay. Ramsay facilities are marked with red crosses. Facilities that have an optimal length of stay and an optimal mortality ratio are clustered near the centre of the graph, close to 1.
In the above, a hospital that has a Risk-Adjusted Length of Stay of 0.5 means that the average length of stay in its ICU is half the predicted length of stay.
What if I don’t want my information to be included in the registry?
Any patient who is eligible for participation in the ANZICS database will be advised by the facility upon their admission to the ICU. If a patient does not want their data contributed, they will need to speak directly to a hospital executive.
Transcatheter Aortic Valve Implantation (TAVI) Registry – ACOR
Transcatheter Aortic Valve Implantation (TAVI) Registry
The Transcatheter Aortic Valve Implantation (TAVI) Registry is a clinical quality registry that monitors the outcomes of patients who have undergone aortic valve replacement via a transcatheter approach.
TAVI is an interventional procedure used to treat aortic stenosis in patients who are deemed as high-risk or inoperable under normal circumstances. Facilities and surgeons who are credentialed to perform TAVI procedures in Australia must follow the guidelines produced by the Australian & New Zealand Cardiac and Thoracic Surgeons (ANZSCTS) and the Cardiac Society of New Zealand.
Any facility that is accredited to perform TAVI procedures must contribute data to the transcatheter aortic valve implantation (TAVI) Registry. The aim of the registry is to improve patient care and outcomes following a TAVI procedure and ensure that all TAVI facilities and surgeons meet their accreditation requirements.
How does participation in this registry assist patients?
Transcatheter aortic valve implantation is a relatively new procedure in Australia. The TAVI registry was established in 2018 and it holds data from 2,462 TAVI procedures that have been performed since then.
As TAVI is a new procedure in Australia, it is critically important to monitor patient outcomes. Any adverse outcomes are monitored and discussed by the multidisciplinary team that performed the surgery.
How do Ramsay outcomes compare?
The following two graphs represent the rate of adverse events in Australian facilities performing the TAVI procedure.
The Ramsay facilities are numbered 4, 5, 24, 27, 38, 41 and 42. The period for this graph is the 1st of July 2019 through to the 30th of September 2019.
View peri-operative adverse events graph.
In this graph the blue bar represents an adverse event before or during surgery: these events are generally classified as cardiac, cerebral, vascular, bleeding, or device related. PPM stands for Permanent Pacemaker – this is something that is typically required after a cardiac event.
The following graph relates to post-operative adverse events. The Ramsay facilities are numbered 4, 5, 24, 27, 38, 41 and 42. The period for this graph is the 1st of July 2019 through to the 30th of September 2019.
View post-operative adverse events graph.
In this graph the blue bar represents an adverse event before or during surgery: these events are generally classified as cardiac, cerebral, vascular, bleeding, or device related. PPM stands for Permanent Pacemaker – this is something that is typically required after a cardiac event.
What if I don’t want my information to be included in the registry?
As a hospital provider accredited to perform TAVI procedures, Ramsay is required to participate in this registry and contribute data. However, any patient who wishes to opt out of the registry can do so. Prior to any surgery, ACOR provides information to patients about the registry, including how to opt out. To date, of the 2,462 cases contributed to the registry, only 42 patients have chosen to opt out.
CARE Network
The Clinical Alliance and Research in ECT and Related Treatments (“CARE”) Network was established by Professor Colleen Loo and her team at the University of NSW in 2015. Seed funding was provided by the NSW Mental Health Commission (MHC) and ongoing support is provided by Chief Psychiatrists in states around Australia. The Network is based at the University of New South Wales and seeks to address translational gaps and unwarranted clinical variation in practice.
The CARE Network is currently focused on ECT, with participating hospitals collecting key clinical data that is used to assess patient outcomes and ensure that facilities are compliant with state-based regulation. As of 2019, the network was made up of 40 hospitals. When Ramsay Health Care joined the network, it grew to more than 55 hospitals.
Four Ramsay sites commenced data collection in July 2020. We anticipate other Ramsay sites will also begin collecting data in the next 12-18 months.
How does participation in the Network assist patients?
ECT is a clinical intervention that can have significant benefit for patients. However, research has also demonstrated that if done incorrectly, the procedure can have a long-term, detrimental effect on cognition. By participating in the CARE Network, Ramsay sites are taking steps to ensure that our ECT services are compliant with state regulation. By actively collecting patient and clinical outcomes in this area, we are also continuously reviewing our ECT services to ensure they continue to deliver high-quality outcomes that benefit our patients.
What if I don’t want my information to be included in the Network?
All patients whose data could be contributed to the Network are provided with an information sheet that explains what the CARE Network is and does, and how their data might be used. Any information that is collected as a part of the CARE Network is de-identified and used for the purposes of assessing the quality of clinical services and overall outcomes for patients.
There is a possibility that any data collected could be used in a research project. If a patient does not want their information used for research, they can opt out following instructions provided in the information sheet.
Ramsay Newsroom
Stay up-to-date with hospital news, developments, research highlights and innovation.